While Rheumatoid Arthritis can pose challenges for dental implant candidacy, it’s not a definitive barrier. In fact, with proper evaluation and care, many patients with this condition can still be suitable candidates for dental implants. Individuals with Rheumatoid Arthritis must consult with their dentist or oral surgeon, who can assess their specific situation and provide personalized recommendations. With appropriate precautions and a comprehensive approach, dental implants can be a viable option for certain RA patients to restore their smiles and improve their quality of life.

Are Rheumatoid Arthritis Patients Candidates for Dental Implants?
Rheumatoid arthritis is a chronic autoimmune disease that primarily affects the joints, causing pain, stiffness, and swelling. It is understandable that individuals with this condition may have concerns about undergoing dental implant surgery. However, with proper evaluation and management, many rheumatoid arthritis patients can be candidates for dental implants.
Understanding Rheumatoid Arthritis and Dental Implants
Rheumatoid arthritis (RA) is characterized by inflammation in the joints, which can lead to joint damage and deformity over time. The disease primarily affects the hands, wrists, and feet, but can also impact other joints, including the temporomandibular joint (TMJ). The TMJ is responsible for jaw movement and plays a crucial role in oral function.
When considering dental implants for rheumatoid arthritis patients, it is essential to evaluate the overall health of the individual, including the severity of their RA symptoms and any related complications. A thorough assessment by a rheumatologist and a dental implant specialist is crucial to determine if the patient is a suitable candidate for the procedure.
Factors to Consider for Rheumatoid Arthritis Patients
1. Disease Activity: The activity level of rheumatoid arthritis is an essential factor to consider when determining the feasibility of dental implant surgery. Patients with well-controlled disease activity may have a higher chance of successful implant placement and integration. However, those with active inflammation and uncontrolled symptoms may need to stabilize theibr condition before proceeding with the procedure.
2. Medication Management: Many rheumatoid arthritis patients are prescribed medications to manage their symptoms and slow down the progression of the disease. Some of these medications, such as corticosteroids and immunosuppressants, can affect the body’s healing process. It is crucial for the dental implant specialist to work closely with the patient’s rheumatologist to ensure proper medication management during the implant placement and recovery period.
3. Oral Health: Good oral hygiene is essential for the success of dental implants in any patient, including those with rheumatoid arthritis. Poor oral health can lead to complications such as infection and implant failure. Regular dental check-ups and thorough oral hygiene practices are necessary to maintain oral health and prevent any potential issues.
4. Joint Involvement: Rheumatoid arthritis can affect the TMJ, causing pain, stiffness, and limited jaw movement. The dental implant specialist should evaluate the patient’s TMJ function and assess if any modifications or adaptations are required during the implant placement process.
The Benefits of Dental Implants for Rheumatoid Arthritis Patients
Dental implants offer several advantages for individuals with rheumatoid arthritis, including improved oral function, enhanced aesthetics, and increased confidence. Here are some key benefits:
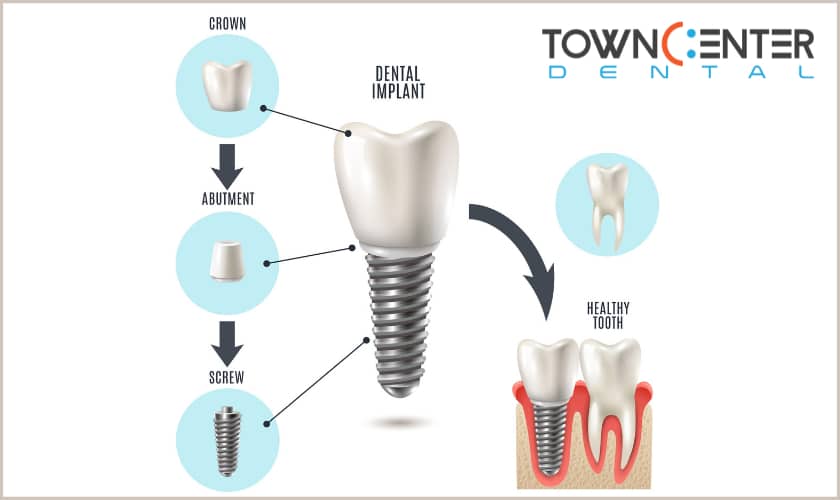
1. Stability and Durability: Dental implants provide a stable and long-lasting solution for tooth replacement. They integrate with the jawbone, mimicking the function of natural teeth. This stability is particularly beneficial for individuals with rheumatoid arthritis, as it can alleviate the discomfort and difficulties associated with loose or ill-fitting dentures.
2. Preservation of Jawbone: When a tooth is lost, the underlying jawbone may start to deteriorate over time. Dental implants stimulate the bone, preventing bone loss and preserving the natural facial structure. This is especially important for rheumatoid arthritis patients, as jawbone health can impact the stability of the TMJ and overall oral function.
3. Enhanced Chewing and Speaking Abilities: Dental implants function like natural teeth, allowing individuals to chew and speak with confidence. This can significantly improve the quality of life for rheumatoid arthritis patients who may experience difficulties with oral function due to joint involvement and pain.
4. Improved Aesthetics: Missing teeth can affect a person’s smile and facial appearance. Dental implants provide a natural-looking solution, enhancing the aesthetics of the smile and boosting self-esteem. This can be particularly beneficial for individuals with rheumatoid arthritis, who may already face challenges related to their condition.
Proper Dental Implant Care for Rheumatoid Arthritis Patients
After dental implant surgery, proper care is essential to ensure the success and longevity of the implants. Rheumatoid arthritis patients should follow these guidelines:
1. Maintain Good Oral Hygiene: Brushing twice a day, flossing daily, and using antimicrobial mouthwash can help prevent infection and maintain oral health. Regular dental check-ups and professional cleanings are also crucial for monitoring the implants’ condition and addressing any potential issues promptly.
2. Manage Rheumatoid Arthritis Symptoms: Staying on top of rheumatoid arthritis treatment and managing symptoms effectively is vital for overall health, including oral health. Working closely with a rheumatologist and following prescribed treatment plans can help minimize the impact of the disease on dental implants.
3. Avoid Excessive Force on Implants: Individuals with rheumatoid arthritis may experience joint pain and stiffness, which can affect their biting and chewing abilities. It is important to avoid excessive force on the dental implants to prevent implant failure or damage. If difficulties arise, consulting with a dentist or prosthodontist for appropriate solutions is recommended.
In conclusion,
Rheumatoid arthritis patients can be candidates for dental implants with proper evaluation, management, and collaboration between medical professionals. By considering factors such as disease activity, medication management, oral health, and joint involvement, dental implant specialists can determine the feasibility of the procedure for individual patients. The benefits of dental implants, including improved oral function, enhanced aesthetics, and increased confidence, can greatly enhance the quality of life for individuals with rheumatoid arthritis. With proper care and maintenance, dental implants can provide a long-lasting and stable solution for tooth replacement in this patient population.
Key Takeaways
- Rheumatoid arthritis patients can be considered as candidates for dental implants with proper evaluation and management.
- Consultation with both a rheumatologist and a dentist is crucial to assess the patient’s overall health and suitability for dental implant surgery.
- Medications used to manage rheumatoid arthritis may affect the healing process after dental implant placement, so close monitoring is necessary.
- Individualized treatment plans should be developed, taking into account the patient’s specific needs and medical history.
- Regular dental check-ups and good oral hygiene practices are essential for the long-term success of dental implants in rheumatoid arthritis patients.
Frequently Asked Questions
Can patients with rheumatoid arthritis get dental implants?
Yes, patients with rheumatoid arthritis can be candidates for dental implants. Rheumatoid arthritis is an autoimmune disease that affects the joints, causing inflammation and pain. However, having rheumatoid arthritis does not automatically disqualify someone from getting dental implants. The decision to proceed with dental implant surgery will depend on the individual patient’s overall health and the severity of their rheumatoid arthritis.
Before undergoing dental implant surgery, it is important for patients with rheumatoid arthritis to consult with both their rheumatologist and their dentist. These healthcare professionals can work together to determine if dental implants are a suitable option for the patient. They will consider factors such as the patient’s level of disease activity, their ability to undergo surgery and heal properly, and any potential complications that may arise due to their rheumatoid arthritis.
Are there any special considerations for dental implant surgery in rheumatoid arthritis patients?
Yes, there are some special considerations for dental implant surgery in rheumatoid arthritis patients. Rheumatoid arthritis can affect the jaw joint, which may potentially complicate the implantation process. Additionally, some medications used to manage rheumatoid arthritis, such as corticosteroids, can affect the body’s ability to heal after surgery.
However, with proper planning and coordination between the patient’s rheumatologist and dentist, these challenges can be addressed. It may be necessary to adjust the timing of dental implant surgery to coincide with a period of lower disease activity. The patient’s rheumatologist can also work with the dentist to develop a medication plan that minimizes the impact on healing while still effectively managing the rheumatoid arthritis.
What precautions should rheumatoid arthritis patients take before dental implant surgery?
Prior to dental implant surgery, rheumatoid arthritis patients should communicate their condition and any related medications to their dentist. This will allow the dentist to assess the potential risks and make any necessary adjustments to the treatment plan. It is important for the dentist and rheumatologist to collaborate and develop a comprehensive approach that takes into account the patient’s specific needs and health status.
In some cases, it may be recommended to have a consultation with an oral and maxillofacial surgeon who specializes in treating patients with rheumatoid arthritis. This specialist can provide further guidance and expertise in managing the unique challenges that may arise during dental implant surgery.
Are there any alternatives to dental implants for rheumatoid arthritis patients?
Yes, there are alternatives to dental implants for rheumatoid arthritis patients. Depending on the individual’s specific circumstances, a removable denture or a dental bridge may be a more suitable option. These alternatives do not require the same level of surgical intervention as dental implants, which may be advantageous for patients with rheumatoid arthritis who may have limitations in their joint function and mobility.
It is important for rheumatoid arthritis patients to discuss all available options with their dentist and rheumatologist to determine the best course of treatment for their oral health needs.
Can dental implants worsen symptoms of rheumatoid arthritis?
No, dental implants themselves do not worsen symptoms of rheumatoid arthritis. However, it is essential to consider the impact of the surgical procedure and the healing process on the overall health of the patient. Any surgical procedure, including dental implant surgery, can potentially cause temporary inflammation and discomfort. It is crucial for patients with rheumatoid arthritis to work closely with their healthcare team to manage any potential flare-ups or complications that may arise during or after the procedure.
By carefully planning and coordinating the treatment with the patient’s rheumatologist and dentist, the risk of exacerbating symptoms can be minimized. Regular follow-up appointments and proper oral hygiene practices can also help maintain the long-term success of dental implants without negatively affecting rheumatoid arthritis symptoms.
Can women with Arthritis opt for Dental Implants? – Dr. Mohammed Fayaz Pasha
Final Thoughts: Are Rheumatoid Arthritis Patients Candidates for Dental Implants?
It is crucial for rheumatoid arthritis patients considering dental implants to consult with both their rheumatologist and their dentist to assess their overall health and suitability for the procedure. With proper evaluation, treatment planning, and collaborative care between the healthcare team, dental implants can be a viable option for restoring oral function and improving quality of life for rheumatoid arthritis patients.
Remember, the decision should be made in close consultation with healthcare professionals who can provide personalized advice based on each individual’s unique circumstances. By taking all necessary precautions and ensuring thorough evaluation, rheumatoid arthritis patients can explore the potential benefits of dental implants and make an informed decision about their dental health.
Call or Book appointment online
:Ace Dental Care Alpharetta office: 678-562-1555 - Book Now
Ace Dental Care Norcross office: 770-806-1255 - Book Now
Disclaimer
This blog post was generated by artificial intelligence. The content of this post may not be accurate or complete, and should not be relied upon as a substitute for professional advice. If you have any questions about the content of this post, please contact us.
We are constantly working to improve the accuracy and quality of our AI-generated content. However, there may still be errors or inaccuracies. We apologize for any inconvenience this may cause.





